It appears that global opinion has been shifting toward a preference for neoliberal policies over the past half century, despite growing inequality in many major economies. Dai Oba (Waseda University, 2020) used an SRG award to advance his research at the University of Oxford to investigate complexities behind this trend among British voters, who appear to have embraced a loosely defined set of attitudes that the author calls “neoliberal folk justice.”
* * *
In May 2023, Onward, a center-right think-tank in the UK, described millennials as “shy capitalists” based on the results of a questionnaire survey. Although millennials are thought to hold egalitarian values and downplay the importance of economic growth and individual effort, Onward found that they also prefer policies of low taxes and less redistribution.[1] This is a good example of how people’s economic views can be quite complex, defying neat categorization into right or left. Similarly to this finding, my research looks into people’s complex views that I call “folk justice”.
In the past half-century, the world seems to have become gradually and increasingly more “neoliberal,” by which I mean an orientation emphasizing the role of the market and associated ideas of the economic right, such as efficiency, personal responsibility, and autonomy. To be clear, most people do not necessarily identify themselves as adhering to a coherent set of beliefs like libertarianism. Rather, many tend to hold beliefs that are loosely defined and not always coherent, which might be described as neoliberal folk justice.
My research is focused on this loosely defined set of attitudes that seems to have a strong and stable hold on a large segment of the population. Increased support for the left, on the other hand, has been relatively rare and short-lived. This is surprising because the comparative merits of egalitarian institutions seem rather indisputable for the majority of the working public, especially in the aftermath of major economic crises in 2008 and 2020. How can this be explained? Is there anything we are not seeing?
As a political philosopher, I am primarily interested in theories of justice and equality. But in analyzing the neoliberal trend, I wished to start with what folk neoliberals on the street believe. Clarity and coherence are extremely important for theories, but people’s beliefs and attitudes can often be unclear and incoherent. So, I wanted to first identify the core beliefs of neoliberal folk justice and build theoretical arguments from the bottom up in the hope they can serve as resources for reasoned democratic deliberation that are accessible to ordinary citizens.
In the following, I will describe my findings of an investigation into neoliberal folk justice, conducted with the help of an SRG award.

People’s deeply held convictions inform their political attitudes. Photo by Dylan Bueltel, https://www.pexels.com/photo/woman-in-red-jacket-holding-a-cardboard-with-message-5233241/.
Complex Attitudes Toward Inequality and Wealth
The complexity of neoliberal-leaning attitudes has been documented by many scholars, whose research reveals some common themes.
Jonathan Mijs, for example, has noted the paradoxical acceptance of inequality in the face of fast-growing inequality and an apparent correlation between such acceptance and levels of inequality. Using International Social Survey Program (ISSP) data covering 23 Western countries and three different periods (1987–88, 1991–93, 2008–12), Mijs tested hypotheses regarding people’s acceptance of rising inequality. He “argue[s] that what explains citizens’ consent to inequality is their conviction that poverty and wealth are the outcomes of a fair meritocratic process.”[2] People’s belief in meritocracy tends to be stronger as society becomes more unequal because, Mijs claims, the affluent and the poor live increasingly separate lives in an unequal society. He posits that greater inequality goes hand in hand with stronger meritocratic beliefs and that stronger meritocratic beliefs, in turn, lead to reduced concerns about inequality.
He also tested the inverse relationships between inequality and notions of structural inequality (that is, lower inequality correlates with stronger awareness about structural factors of inequality, and stronger beliefs about structural inequality correlate with greater concern about inequality). He confirms the hypothesis, with the effect of meritocratic beliefs being stronger than the effect of beliefs in structural inequality. Mijs’s key finding is that economic inequality tends to be seen as acceptable when people believe their society embodies meritocratic principles, a belief which, in turn, is strengthened by a rise in inequality.
While Mijs’s findings suggest links with the idea of procedural justice, the notion of meritocracy is a vague one. In fact, Mijs construes meritocratic beliefs rather narrowly as people’s belief in the importance of hard work as a factor for economic success. There can be some variety in what people mean by the “importance of hard work” ranging from, for example, hard work in employment and non-paid work to being responsible and prudent in managing their finances and “giving back” to society.
Regarding what makes inequality (appear) legitimate, Rachel Sherman conducted interviews with 50 wealthy couples in New York and found that the affluent feel a strong need to be able to justify their wealth. Her interviewees had household incomes within the top 5% in New York City—the most unequal large city in the US—and were characterized as the “new elite” who “believe in diversity, openness, and meritocracy rather than status based on birth.”[3] To Sherman’s surprise, many affluent New Yorkers expressed moral conflicts about their privilege and shared various narratives to demonstrate their worthiness, which she broadly categorized into three types.
The first narrative is that of the hard worker marked by such redeeming qualities as productivity, self-sufficiency, discipline, and independence. The second narrative is that of the prudent consumer. The rich New Yorkers cast themselves and their spending habits as “normal” in an attempt to distance themselves from the negative image of the “leisure class.” In line with the Protestant ethic, disciplined spending is considered part of the meritocratic ideal and thus a legitimator of their wealth. The third narrative is that of someone actively “giving back” to society typically by donating their money or time to charitable organizations.
We can see certain aspects of folk neoliberal values underlying these research findings, namely, the idea of meritocracy, under which economic success is ascribed to an individual’s personal merits; the value placed on hard work over idleness and dependence; the ideal of prudence and responsibility; and the imperative of “giving back” to society.
Four Values of Neoliberal Folk Justice
Rather than describing the minute details of people’s complex attitudes, I focused on the following two claims as being the core beliefs of neoliberal folk justice, namely, that redistribution is unfair and that government should not intervene in the market.
These claims can be unpacked into the following four normative values. First, social cooperation should be on a quid pro quo basis, and freeriding should not be allowed. This requires that there is a certain equity between contributions and benefits. Second, those who rely on welfare do not deserve further assistance because they lack a sense of personal responsibility. This claim points to a personal virtue of using of resources (including time and talent) in a prudent and thoughtful manner. Third, market outcomes are morally fair. This can be understood as an expression of trust in the market mechanism and its ability to legitimate distributive outcomes. Fourth, each person is the sole author of his/her life, and the government should not interfere or even offer any help. This expresses the moral ideals of self-sufficiency, independence, and, most importantly, the ability to advance one’s life as his or her own project and no one else’s.
In sum, the four core values of neoliberal folk justice are (1) reciprocity, (2) responsibility, (3) procedural fairness, and (4) autonomy.
Survey Findings

What do people believe about just economic policies? Photo by Karolina Grabowska, https://www.pexels.com/photo/quote-board-on-top-of-cash-bills-4386367/.
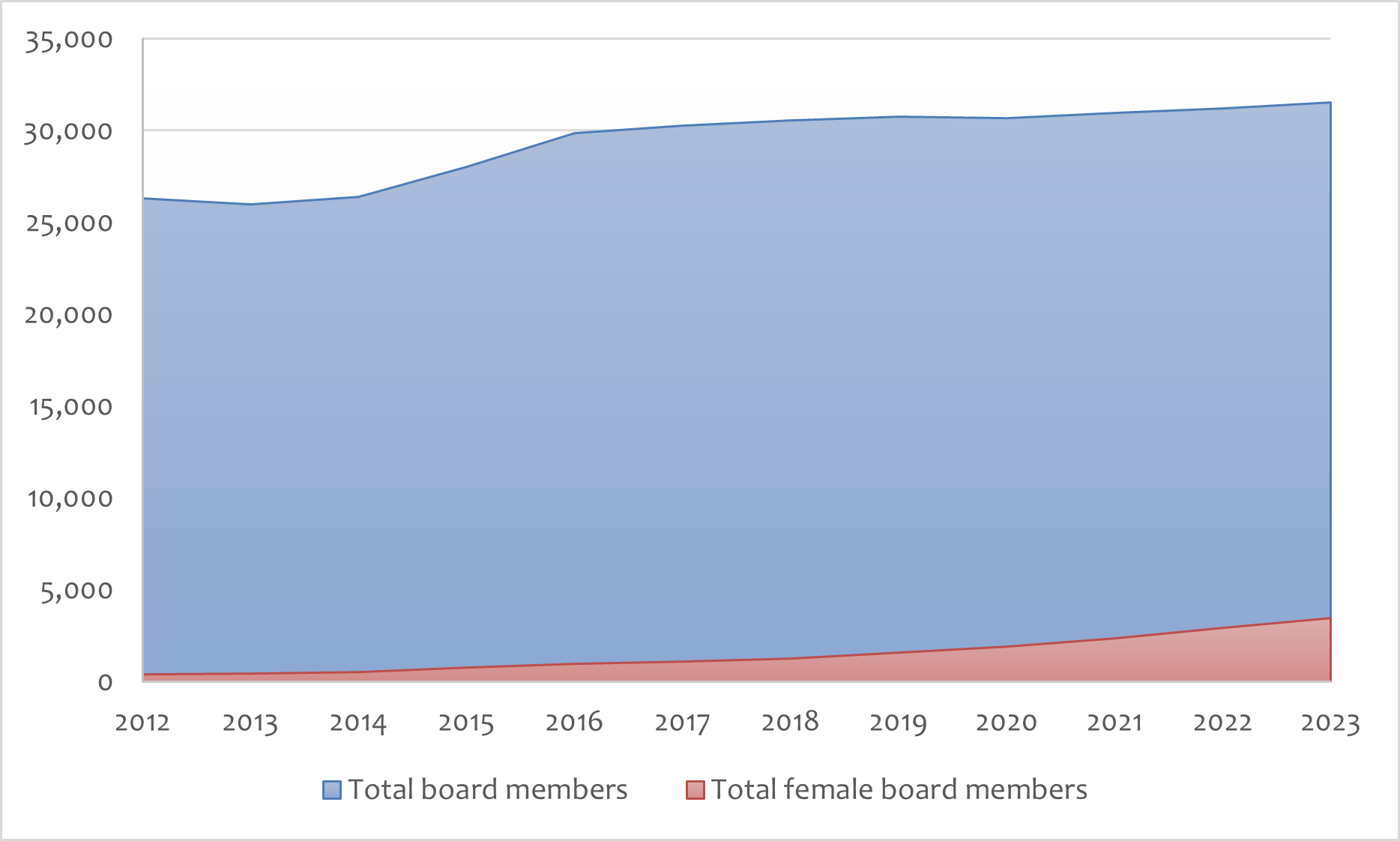
I conducted an online opinion survey of 2,065 adults living in Great Britain (England, Scotland, and Wales) to directly test the above selection of core values. Along with two dummy values (“solidarity” and “efficiency”) and after explaining what each value stands for, I asked respondents to rate the importance of the four values when thinking about economic policies that are fair for everyone (respondents were asked to select from ‘very important’, ‘fairly important’, ‘not very important’, ‘not at all important’, and ‘don’t know’).
The results of the survey confirmed my selection of the above four values. Comparing the percentages of those who answered “very important” or “fairly important,” the four values all scored 70% or higher (79% for “procedural fairness,” 78% for “responsibility,” 71% for “reciprocity,” and 70% for “autonomy”), while the dummy values scored significantly lower (59% for “efficiency” and 58% for “solidarity”). Additionally, correlations with respondents’ past voting behavior revealed that for both the 2015 and 2019 general elections, those who voted for the Conservatives supported the four values significantly more than those who voted for Labour (the difference ranging from 10 percentage points to 30 points). This supports my hypothesis that the four values have particularly strong resonance with folk neoliberals.
Toward Theoretical Arguments and Policy Consensus
Based on the above findings, the next stage of my research will offer repertoires of theoretical arguments regarding the four values of neoliberal folk justice, each of which represents a potential salient political position that citizens may adopt. As a final output, I aim to describe potential areas of policy consensus between those different arguments, showing that reaching an agreement on desirable and feasible social welfare policies for the twenty-first century is a realistic possibility.
[1] Jim Blagden and Sebastian Payne, “Missing Millennials,” Onward, May, 2023, https://www.ukonward.com/wp-content/uploads/2023/05/missing_millennials-1.pdf, accessed 19 October 2023.
[2] Jonathan Mijs, “The Paradox of Inequality: Income Inequality and Belief in Meritocracy Go Hand in Hand,” Socio-Economic Review, vol. 19, no. 1: 7–35 (January 2021), p. 29.
[3] Rachel Sherman, Uneasy Street: The Anxieties of Affluence, Princeton University Press, 2017, pp.13–15.